Breast Cancer
Breast Cancer
Being diagnosed with breast cancer is very frightening. Understanding the different types of cancer, is the first step in understanding treatment options. The discussion of breast cancer is multidisciplinary. The focus of treatment options and, insight into many aspects of breast cancer treatment is paramount to making informed decisions. These treatments may include surgery, radiation therapy, chemotherapy, hormonal blockade, and genetic testing.
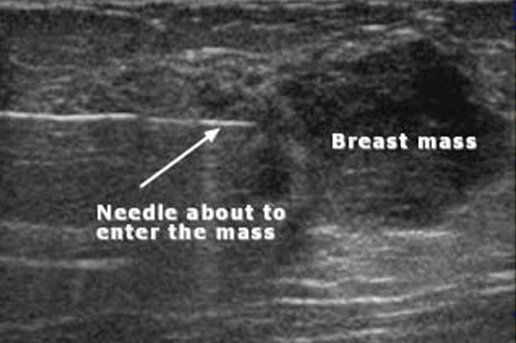
Breast Biopsy
Breast biopsies are sometimes required to make a definitive diagnosis. If the lesion of concern is too small to appreciate by ‘feel’, a needle localization may be necessary. Needle localization, is done in the Breast Imaging Department. A mammogram or ultrasound (sometimes an MRI) is used to identify the lesion of concern, and, then to guide a wire, placed next to (adjacent) to this area of concern. This localizing wire, will assist surgically, in identifying the area of concern.
Subareolar dissection is a procedure that is sometimes performed in women who have unexplained nipple discharge. This is a procedure, whereby, the affected (draining) duct is isolated and a portion removed. Similar to a breast biopsy, the procedure sometimes requires a preoperative localization. Although most nipple discharge is from a benign (noncancerous) etiology, biopsy/subareolar dissection is at times required.
Imaging and Diagnostic Procedures
There are multiple imaging modalities utilized in diagnosing disease of the breast: breast ultrasound, breast MRI, tomosynthesis or 3D mammography, image guided core needle biopsies (ultrasound, MR, and, stereotactic guided), as well as, less conventional studies like thermascan. The goal of diagnostic imaging and biopsy is to utilize the least invasive technique to make a definitive diagnosis. The most critical part of making a diagnosis, is determining the appropriate testing needed. Just because there ‘is a test’ doesn’t mean it is necessary. The right test for the right patient is paramount to high quality care.



